School of Pharmacy Professor Michelle Chui publishes the first study on the implementation of CancelRx, which showed a 93% success rate in canceling prescriptions from the clinic to the pharmacy at UW Health
By Katie Ginder-Vogel
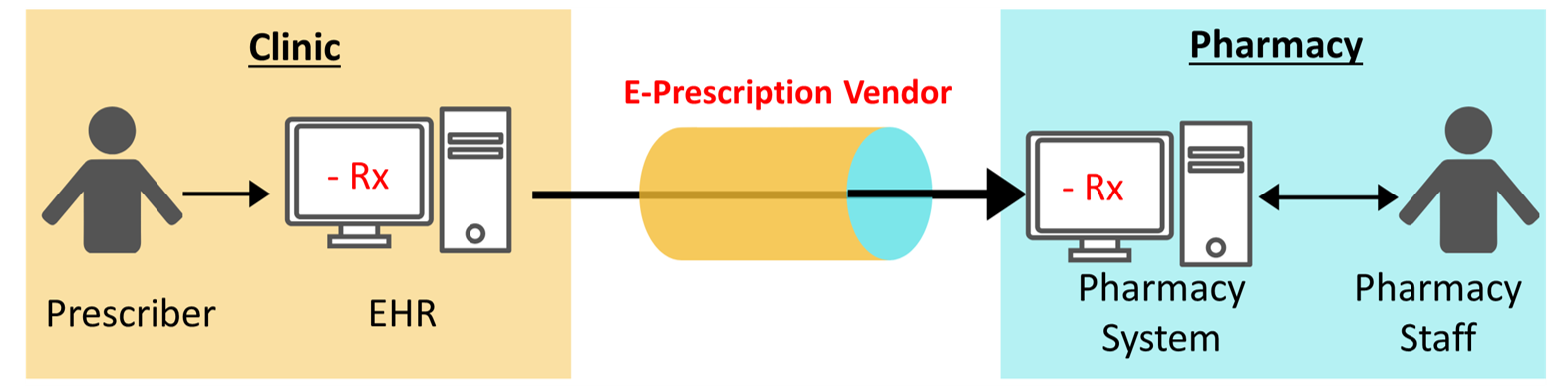
When a doctor stops or changes a prescription in a patient’s electronic health record, this information may not reach the pharmacy, leading to the problem of dispensing discontinued medications. A new study from a team of researchers at the University of Wisconsin–Madison has found that the e-prescribing tool CancelRx more than doubled the proportion of successfully discontinued medications, from 34 percent to 93 percent, at UW Health, a major health system in Wisconsin.
CancelRx, built and standardized by the National Council for Prescription Drug Programs (NCPDP), is the only tool of its kind. Without CancelRx, there is no automatic mechanism to notify pharmacies of canceled prescriptions, leaving the door open for patients to be over-prescribed or to pick up discontinued medications, both of which pose a health risk.
The findings could encourage more health systems to utilize CancelRx to improve patient safety.
The researchers, led by UW–Madison School of Pharmacy Professor Michelle Chui, reviewed data comparing the 12 months preceding UW Health’s implementation of CancelRx in October 2017 to the 12 months following implementation.
“This research project presented an opportunity to implement a healthcare technology at an academic health center and use the data to demonstrate that, on a really large scale, CancelRx was successful at deactivating medications in the pharmacy that had been discontinued by the provider,” says Chui.
Their findings — the first peer-reviewed study into a health system-wide implementation of CancelRx — were published in the Journal of the American Medical Informatics Association on April 9.
“CancelRx has been around since 2017, and even so, there are many health systems that have not turned it on,” says Chui. “CancelRx is intended to improve medication safety in outpatient settings. Our findings on the successful implementation of CancelRx could potentially push health systems to move forward on this.”
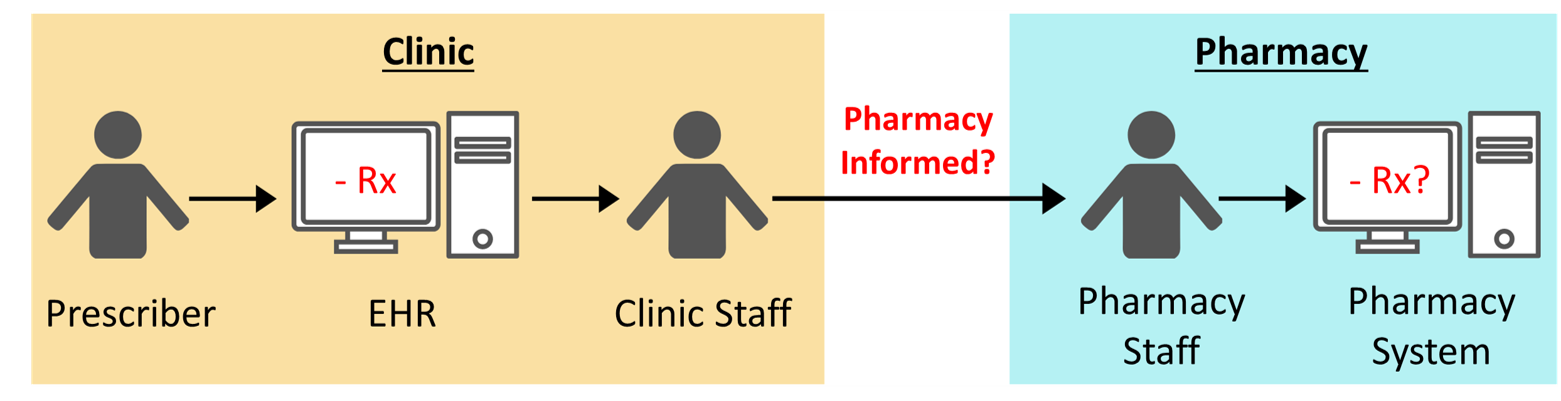
The greatest change in the proportion of successfully discontinued medications was in primary care settings, a 71 percent increase, as compared with specialty care, which increased 54 percent. Before CancelRx implementation, it took an average of 12 hours for clinic staff to manually contact pharmacies about a canceled medication — sometimes several days, depending on clinician workflow. With the tool, the communication is immediate.
“This has the potential to increase patient safety by improving communication and ensuring things don’t fall through the cracks,” says study coauthor Taylor Watterson, a graduate student in the School of Pharmacy’s Health Services Research in Pharmacy program.
“It has safety implications for controlled substances, including opioid pain medication, stimulants, and benzodiazepines,” she says. “A patient could have multiple prescriptions on file in multiple places, and it can be hard to track, so technology like CancelRx has a practical safety application in those situations, too.”
In addition to Chui’s research group at the School of Pharmacy, the study authors reflect collaborators with diverse expertise from across the UW–Madison campus — including the School of Medicine and Public Health, College of Engineering, and the School of Nursing — as well as the Wisconsin Department of Health Services and the Johns Hopkins University School of Medicine.
“This is a great collaboration between the School of Pharmacy, UW Health, and the UW School of Medicine and Public Health,” says Chui. The research was funded by the Agency for Healthcare Research and Quality, The Gordon and Betty Moore Foundation, the National Council for Prescription Drug Programs Foundation, and the UW–Madison Office of the Vice Chancellor for Research in Graduate Education.
More research opportunities to enhance pharmacists’ role in patient safety
Going forward, the project lays the groundwork for future research.

For example, researchers can explore how the tool affects the workflow of both clinicians and pharmacists and how CancelRx would work at community pharmacies outside of a health system, such as Walgreens, CVS, or an independent pharmacy.
CancelRx notifies pharmacists that a medication was stopped, but not why it was stopped, so Watterson sees an opportunity for researchers to explore that question, too.
“If a medication is stopped for an anaphylactic reaction, that’s more serious than just wanting to stop it because another medication worked better,” she says. “If pharmacists know why, then they have access to the patient care process, which improves coordination of care.”
As one of the most accessible providers, pharmacists can impact patient health by ensuring medication safety.
“We saw the lifecycle of the prescription, all the way from the physician’s office to the pharmacy,” says Chui. “Ultimately, we want to equip pharmacists with the right information, so they can take care of their patients. This is just one demonstration of how that can be done.”