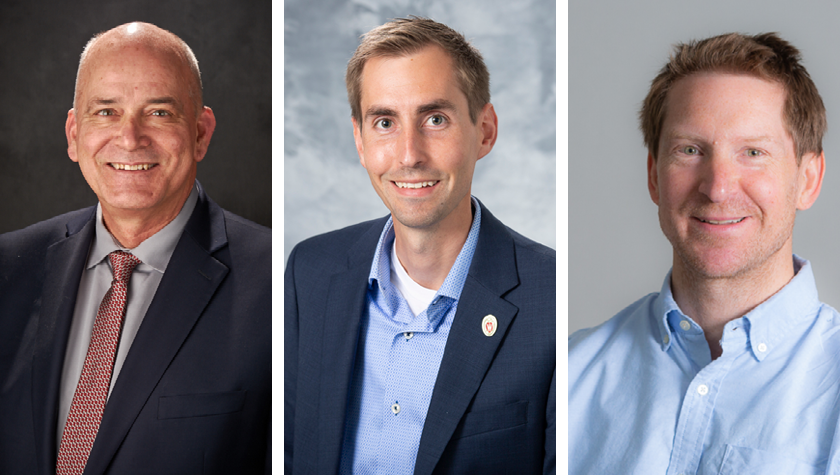
Professor Paul Hutson and collaborators in the Transdisciplinary Center for Research in Psychoactive Substances study psilocybin for opioid and methamphetamine use disorders
By Katie Gerhards
Three million people in the U.S have or have had opioid use disorder, and another 1.5 million people have dealt with methamphetamine misuse, within the last year alone.
But two new groundbreaking clinical trials out of the UW Transdisciplinary Center for Research in Psychoactive Substances (TCRPS), housed within the University of Wisconsin–Madison School of Pharmacy, aim to address these pressing issues with a promising psychoactive agent: psilocybin.
The drug has so far shown promising results for patients with mental health concerns such as depression and tobacco and alcohol misuse. Now, a UW–Madison research team is investigating the use of psilocybin to aid in decreasing opioid and methamphetamine misuse.
The team includes Paul Hutson — professor in the School’s Pharmacy Practice and Translational Research Division and founding director of the TCRPS — as well as Randall Brown and Christopher Nicholas, faculty in the UW School of Medicine and Public Health.
“We already have evidence that psilocybin can do some remarkable things to improve the patient’s ability to gain and process important insights about their lives and experiences.”
—Paul Hutson
The clinical trials underway for both opioid and methamphetamine use disorder represent groundbreaking firsts in their use of psilocybin and in their flexible design.
“We already have evidence that psilocybin can do some remarkable things to improve the patient’s ability to gain and process important insights about their lives and experiences,” says Hutson, a co-investigator on both studies. “We’re excited to see what it can do along those same lines for patients struggling with substance abuse, many of whom have overlapping mental health conditions.”
Rethinking study design
Both the methamphetamine and opioid trials are open-label, single-arm trials, meaning there is no control group or placebo involved. The goals of the trials are purely to test for safety and feasibility — once established, this groundwork will allow for future studies about the effectiveness of the treatment.
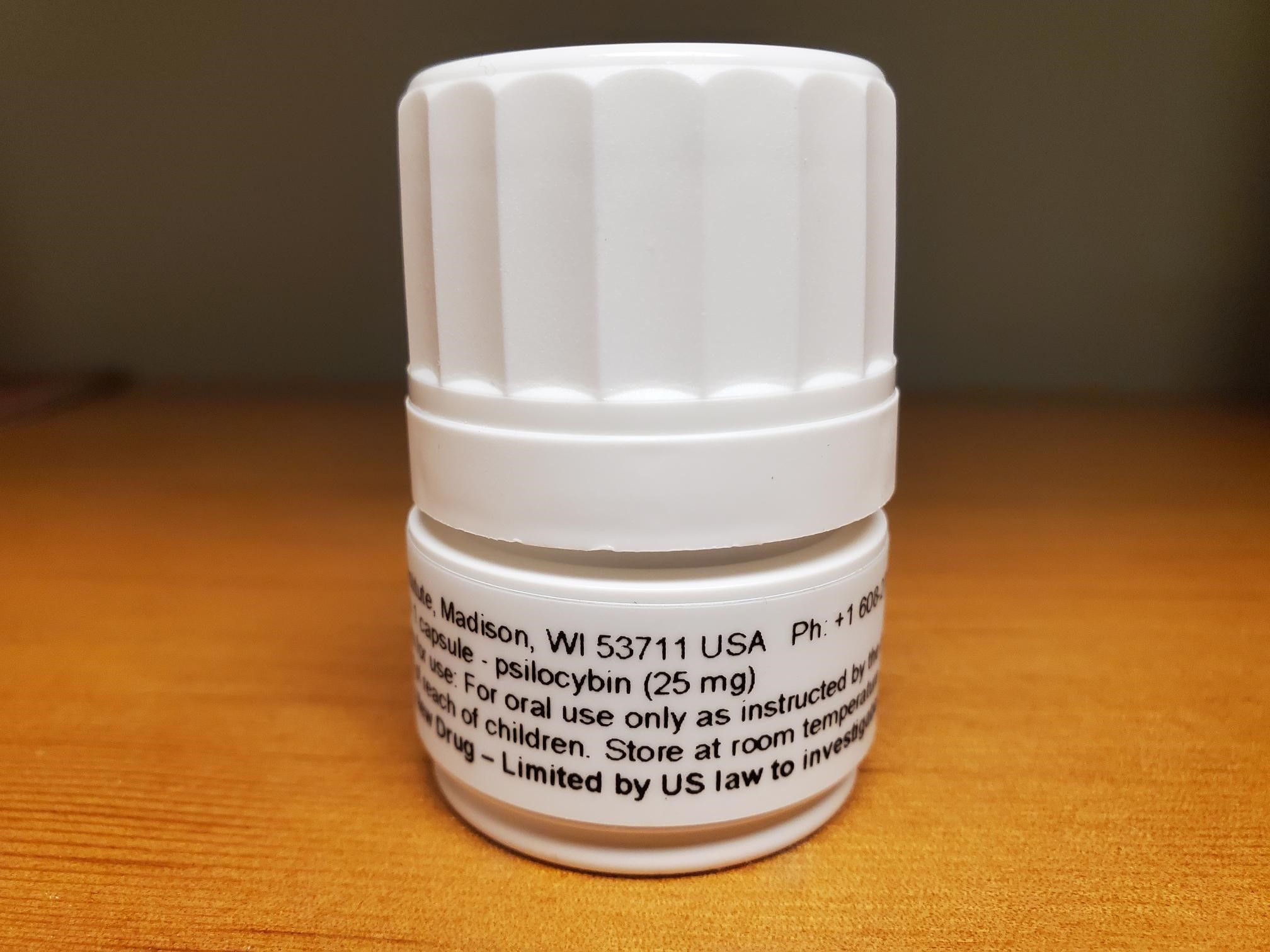
Every participant in these trials will undergo a psychological screening and at least six hours of preparatory counseling. With the preparation complete, participants receive at least one 25 milligram dose of psilocybin and will then be observed for eight hours by two therapists in the School of Pharmacy’s dedicated Clinical Research Facility — an unparalleled space that largely resembles a living room, decked out with the comforts of home plus monitoring technology to ensure study replicability.

After the eight hours of monitoring, participants spend the night in the Clinical Research Unit at the UW Health hospital, followed by an integration or debriefing session with a psychologist before they’re discharged, which helps them process their experience for maximum benefit.
“To be optimally therapeutic, psychedelic drugs need to be integrated with an adequate preparation and screening of patients to confirm that they are appropriate to receive these medications, that they are attended by trained therapists, and that they then have one or more integration sessions afterward so they can have some guided interpretation of their experience,” says Hutson. “We also recognize the need to provide subsequent support of the patients to reinforce desired behavioral and lifestyle changes. That can be a challenge in this patient population.”
Four weeks after the first dose, participants will have the option to take a second dose of either 25 or 50 milligrams, based on whether they received an adequate psychedelic experience the first time.
“A component that’s remarkably different than other psilocybin studies is this option of increasing the dose, for both the opioid and methamphetamine studies,” says Hutson. “That’s uncommon and will test the idea of whether there’s a dose response to outcomes from psychedelics.”
Participants in drug trials often face stringent eligibility criteria, but the UW–Madison team is rethinking some of the historic exclusionary conditions in favor of including persons more representative of those abusing opioids or methamphetamine.
“We’re getting into populations that are pretty cutting edge for substance use disorder trials,” says Brown. “We’re sort of building the plane as we fly it on some fronts.”
“We’ve developed the idea that the experience occasioned by psilocybin may lead to thinking differently about the value of treatment and the value of positive behavior change around their substance use.”
—Randall Brown
“If we’re going to recruit a sample of patients that’s more helpful to clinical practice in terms of how generalizable it is, we need to do careful thinking about this balance of eligibility, and what issues are likely to affect safety,” says Brown. “For example, with patients who also have ADHD, we reframed the inclusion criteria to allow them to be eligible if they can taper off that medication within a reasonable time before the dosing session.”
Participants’ final follow-up visit is two months after the last dose, at which time patients will be evaluated not only on their psychedelic experience, but also about how their substance use has been impacted, such as less frequent use or craving to use, or a change in how they perceive their misuse.
Unique challenges of substance misuse
Historically, clinical trials addressing methamphetamine use disorder have a high attrition rate, meaning participants don’t stick with the program, compromising the results and adding an additional barrier to finding effective therapies.
“Methamphetamine has a quite high attrition rate compared with other clinical populations — about 50 percent drop out of clinical trials of pharmacological and behavioral treatments — so we wanted to make sure that our study design was adapted to support their needs,” says Nicholas, the principal investigator on the methamphetamine study, which is being funded through a partnership with Revive Therapeutics.
Clinical trials are quite rigorous and time consuming, he says, so these two studies are designed to offer as much flexibility as possible, such as the option of receiving one or two doses and the option of a higher second dose.
Starting later this year, the team is recruiting individuals who are actively using methamphetamine — another aspect of the study that breaks new ground.
Typically, participants in substance misuse trials have detoxed and been stabilized. In this clinical trial, studying active users will enable the researchers to take a closer look at how addiction and psilocybin impact the brain through MRI scans. Scans will be taken before and after each psilocybin dose to acquire some early data on how functional networks in the brain associated with addiction, mental health, and well-being may change across the course of the study.
“We’ll hopefully be able to correlate these changes in various outcome measures, whether it’s mood, addiction-related constructs, well-being, or emotional measures,” says Nicholas.
They also built in a therapeutic protocol that combines features of motivational interviewing, emotion-focused, and mindfulness-based therapies as a unique harm-reduction approach.
“These therapies are integrated within an ‘inner-directed’ approach to using the psilocybin,” says Nicholas. “This is a way for us to assess how illicit drug use changes and if it can be reduced, and so that the individual can learn more about their addiction and the factors within their life that may contribute to their addiction.”

“We’ve developed the idea that the experience occasioned by psilocybin may lead to thinking differently about the value of treatment and the value of positive behavior change around their substance use,” says Brown.
The clinical trial exploring psilocybin for opioid use disorder, led by Brown and funded by the Heffter Research Institute and a gift from the Etheridge Foundation, also marks new territory.
“The opioid use disorder study is really the first of its kind,” says Brown. “There hasn’t been any study of psilocybin in the setting of opioid use disorder.”
Studying those who misuse opioids requires some additional considerations for safety because of risks associated with overdose and mortality that go along with fentanyl and analogues in supply, Brown says. Preventing withdrawal symptoms with buprenorphine can help individuals avoid using far riskier street drugs.
“Part of the opioid study protocol involves stabilizing individuals on a buprenorphine product to prevent complications along those lines,” says Brown.
New horizons
The opioid use disorder study got underway in 2021, and the methamphetamine use disorder study is ready to begin recruitment. Although both studies are in their early stages — estimated to wrap up in mid to late 2023 — the research team is looking downstream at how these studies may add to the scientific and cultural understanding of psilocybin and what areas of research are next.
One of the myths they hope to dispel as research advances in the area of substance misuse is that a treatment with psilocybin is simply trading one drug for another.
“There’s no evidence that psilocybin and LSD are addictive agents,” says Hutson. “People do not have a craving to keep taking them like they do alcohol, tobacco, or opioids.”

And despite encouraging findings across a range of conditions — including depression and post-traumatic stress disorder — the clinical environment, not just psychedelics themselves, is key to patient success.
“They’re not a quick fix,” says Nicholas. “They have the potential to be very helpful for a number of mental health and substance use disorders, but it’s a full package treatment that involves counseling before and after to prepare for and make sense of these experiences.”
As the methamphetamine and opioid clinical trials aim to establish the safety and feasibility of the psilocybin intervention, the team plans to use their findings to apply for federal funding for larger clinical trials into the efficacy of the treatment.
In the meantime, they’re hoping to tackle a new arena: stroke recovery. Their stroke work, if funding is secured, would work on two goals: One aim would be to see whether psilocybin could help treat depression, which affects an estimated one in three stroke survivors. Another is to investigate the drug’s ability to speed the healing of the brain itself.
“We want to evaluate whether healing is accelerated with the addition of psilocybin,” says Hutson. “We think that might be the case because there are data that suggest there is an enhancement of neuronal regrowth or additional synapses that are created in mouse models of psychedelic dosing.”