The team’s winning paper explores impactful changes to pharmacist and prescriber workflow
By Aarti Gupta
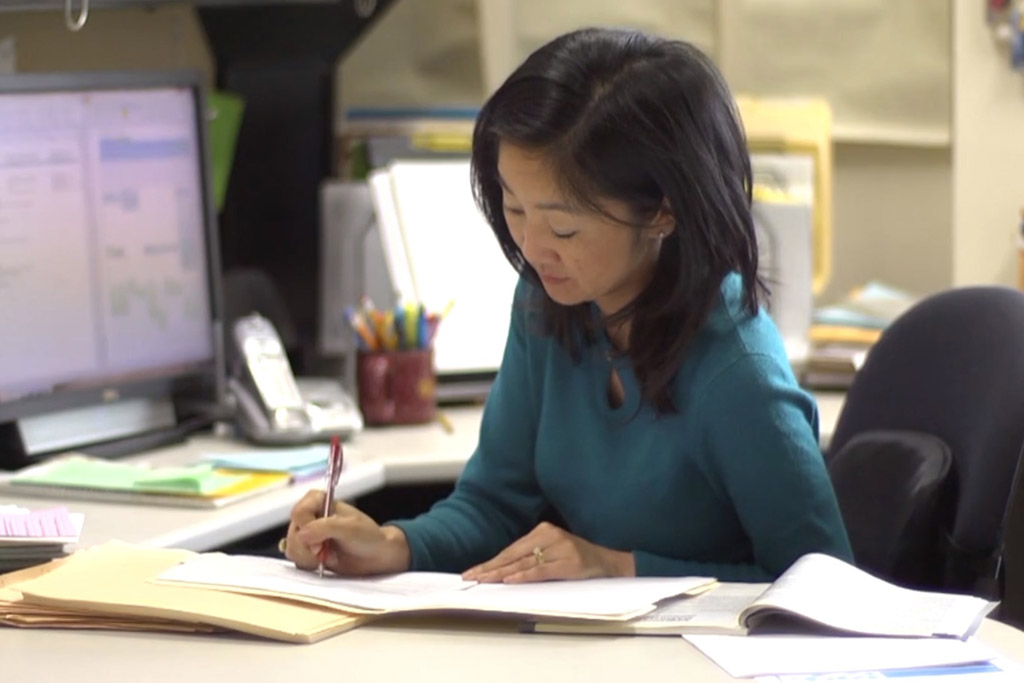
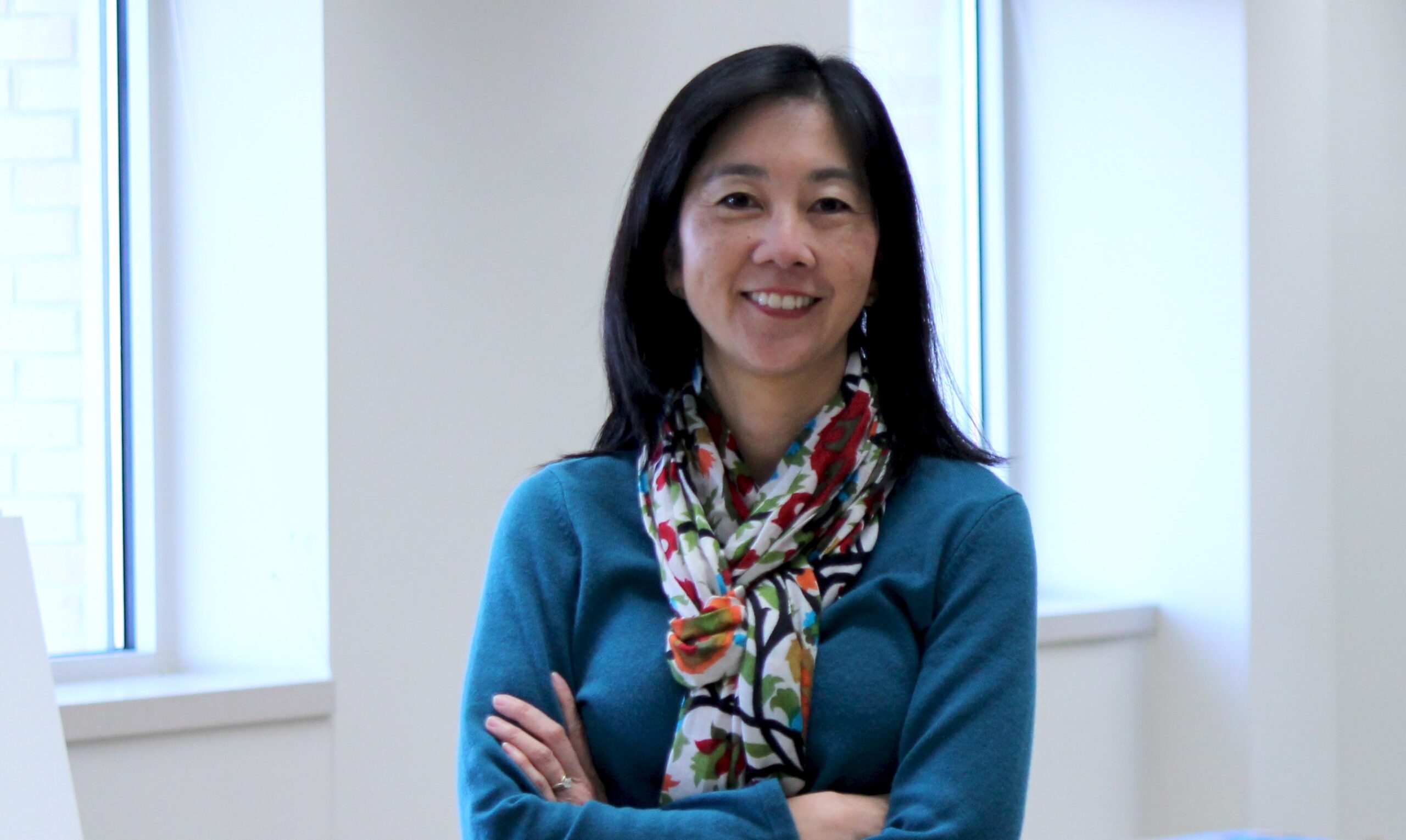
“Picture a community pharmacy where there’s a drive-thru window, two checkout windows, and pharmacists and technicians that are moving around,” says Michelle Chui, professor and chair of the University of Wisconsin–Madison School of Pharmacy’s Social and Administrative Sciences Division. “Nothing is very linear, even though it’s supposed to be, so the workflow is very complicated and opaque. It’s not very clear what people are always doing all the time.”
Starting in 2017, Chui and her research group — the Chui SAMS (Systems Approach to Medication Safety) Lab — led a groundbreaking study into a tool designed to improve pharmacy workflow and improve patient safety in the process. That tool was CancelRx, a technology that electronically sends cancellation messages to pharmacies about medication changes or discontinuations.
By studying the implementation of CancelRx at UW Health — the first study of a health system-wide implementation of the tool — Chui’s group found that the technology successfully improved the rate of prescription cancelations discontinued at the pharmacy. Prior to the implementation of CancelRx, only 34 percent of prescriptions were discontinued. In sharp contrast, after the implementation of CancelRx, that portion leapt to 93 percent.
“Personally, I am a ‘strident fan’ of workflow redesigns and implementation of other programs that can ameliorate the administrative workload of pharmacy staff, thereby reducing burnout and improving safety.”
—Shane Desselle
But their work didn’t end there. With Taylor Watterson (MS ’18, PhD ’22), then a graduate student in the School’s Health Services Research in Pharmacy (HSRP) program, scientist Aaron Gilson, researcher Jamie Stone, HSRP graduate student Sara Hernandez, and collaborators at UW Health, Chui continued evaluating the impact of the tool on pharmacist and prescriber workflow.
Their findings, published in the journal Exploratory Research in Clinical and Social Pharmacy (ERCSP), are so significant that the paper earned ERCSP’s 2022 Best Paper of the Year award.
“The panel of judges voted for it unanimously among the papers that were nominated for the award,” says Shane Desselle, editor of ERCSP. “Personally, I am a ‘strident fan’ of workflow redesigns and implementation of other programs that can ameliorate the administrative workload of pharmacy staff, thereby reducing burnout and improving safety. I hope that this paper generates some much-needed conversation and additional research.”
Workflow changes
Looking back to 2017, Chui says her group was fortunate to be able to partner with two physicians at UW Health, who were leading the CancelRx implementation.
“UW Health took a chance to implement this, and we were along for the ride to evaluate it,” says Chui. “Our goal was to evaluate cost, workload, and safety to demonstrate that CancelRx could lead to positive work and reduction in workload, hopefully, and share that with other health systems and community pharmacies considering adopting it themselves.”
Watterson, lead author on the study who is now a postdoctoral research fellow in the UW Department of Family Medicine and Community Health, says her curiosity to pursue this project stemmed from a motivation to improve pharmacists’ workload.
“CancelRx is an intervention that seemed really tangible and really easy,” she says. “And so the fun part was trying to figure out what isn’t as easy as it should be. Where can we poke holes in this process to make sure that we’re making sure it’s as safe as possible and improving the work and care that pharmacists are able to provide?”

Community pharmacies are inherently complex systems, between demand for tests, vaccines, prescriptions, consultations, and more. Manual prescription cancelations add another layer to this work — and with it, a vulnerability for errors.
Prior to the implementation of CancelRx, canceling prescriptions could be divided into a six-step process, starting with the prescriber.
Peter Kleinschmidt, a physician at UW Health, says that before CancelRx, when he would enter a canceled prescription into the patient’s electronic health record, he was prompted to say why. Then, it fell on nurses, medical assistants, and other staff to call the pharmacy, who could take moments or days to relay the message, depending on their workload.
“Just having the time to pick up the phone and call creates a bigger barrier,” says Kleinschmidt.
The pharmacist would then receive the message, from the prescriber’s office or from a patient, which would lead them to investigate the change to verify it with the patient’s profile and prescriptions. They then had to manually discontinue the prescription by deactivating it in the system and document any information related to the discontinuation. Lastly, the pharmacist would communicate the medication changes with any other staff members or the patient.
“We wanted to investigate how we automate something to make it more standardized, more transparent, more reliable, to then help pharmacists do the job that they want and need to do.”
—Michelle Chui
“Human beings are busy,” says Chui. “Things fall through the cracks, or those phone calls get delayed. We wanted to investigate how we automate something to make it more standardized, more transparent, more reliable, to then help pharmacists do the job that they want and need to do.”
After implementation, CancelRx would automatically receive, match, discontinue, and communicate any changes to the prescription within the patient’s record. If the system was not able to match the prescription, CancelRx would notify the prescriber to follow up with the pharmacy about the prescription for manual updates. However, in more than half of the cases studied, pharmacists did not need to further investigate the CancelRx discontinuations.
“With CancelRx, I can confidently know that when I’m stopping a medication in the clinic, the pharmacy will be immediately prompted to not distribute it,” says Kleinschmidt.
Enhancing patient care
Although workflows are changing behind the scenes, the only difference for patients will be the improved safety and accuracy of their prescription orders.
“The beauty of CancelRx is that it’s something that works behind the scenes to help prescribers and pharmacists improve patient safety, while being pretty much invisible to patients,” Chui shares.
Now, with real-time prescription updates between prescribers and pharmacies, there are fewer discrepancies, which takes some pressure off the patient’s shoulders.

“This automated system makes it easier on my patients, too. Sometimes, they can struggle to understand what medication they should be taking, or I give them a note with instructions to share with their pharmacist,” says Kleinschmidt. “That’s an incredibly vulnerable process, and CancelRx helps to eliminate that vulnerability.”
The School’s pioneering research has led CancelRx to be applied in over 70 percent of health systems in the United States — a number which Chui, Watterson, and Kleinschmidt hope will increase to 100 percent in the near future. However, CancelRx isn’t the only project the School is developing to change the workflow in pharmaceutical practices.
Currently, Watterson and Kleinschmidt are coinvestigating a new project called RxFill, which streamlines the flip side of pharmacy-prescriber communications: It sends information from the pharmacy to the clinic to notify the doctors that the prescription has been filled.
“Like this project with CancelRx showed, there’s no real communication between pharmacies’ and clinics’ patient records,” says Watterson. “This is the next step in creating a volley of messages between these two systems.”
The CancelRx study provides a foundation that shows how pharmacists and providers can adapt technology to increase patient safety and streamline their work, freeing up time to focus on patient-oriented tasks.
“The beauty of healthcare is that there’s human beings involved. It’s not robots,” says Chui. “Human beings can evolve and make things more efficient, and what this paper did is demonstrate the evolution of how pharmacists adapt to interventions like technology. We can use this study as a roadmap for exploring the healthcare workflow and making further impacts.”